Advanced Cell Technology, Inc., a biotechnology company applying cellular technology in the field of regenerative medicine, announced today that the U.S. Food and Drug Administration (FDA) has granted orphan drug designation for the company’s MA09-hRPE cells for use in the treatment of Stargardt’s Macular Dystrophy (SMD).
“We are pleased that the FDA has, for the first time, granted orphan drug status for the use of an embryonic stem cell derived therapy in treating an unmet medical need,” said Edmund Mickunas, Vice President Regulatory. “We believe that our terminally differentiated RPE cells represent a promising treatment for patients with SMD and expect to be in a position to accelerate clinical development and hopefully make RPE cellular therapy available to the majority of patients sooner.”
US orphan drug designation is granted to companies with products aimed at treatment of a rare disease or condition that affects fewer than 200,000 Americans. The National Institutes of Health (NIH) recently proposed broadening the definition of a human embryonic stem cell to include ACT’s “single blastomere technology platform” which was used to derive ACT’s MA09-hRPE cells. The Company believes that the SMD program should be eligible for federal funding once the change is published in the Federal Register.
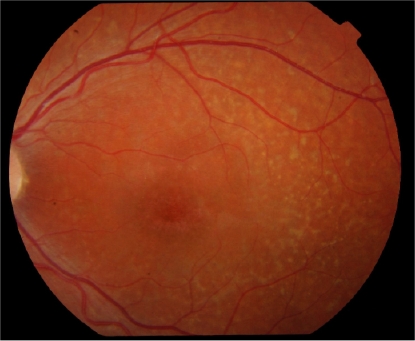
Degenerative diseases of the retina are among the most common causes of untreatable blindness in the world, and as many as ten million people in the United States have photoreceptor degenerative disease. While most of these patients have Age-Related Macular Degeneration (AMD), a smaller number have Stargardt’s, an Orphan disease and to date an untreatable form of juvenile macular degeneration leading to blindness in a much younger group of patients than are affected by AMD. ACT’s treatment for eye disease uses stem cells to re-create a type of cell in the retina that supports the photoreceptors needed for vision. These cells, called retinal pigment epithelium (RPE), are often the first to die off in SMD and AMD, which in turn leads to loss of vision.
While there is currently no treatment for SMD, several years ago ACT and its collaborators discovered that human embryonic stem cells could be a source of RPE cells. Subsequent studies found that the cells could restore vision in animal models of macular degeneration. In a Royal College of Surgeons (RCS) rat model, implantation of RPE cells resulted in 100% improvement in visual performance over untreated controls, without any adverse effects. The cells survived for more than 220 days and sustained extensive photoreceptor rescue. Functional rescue was also achieved in the ‘Stargardt’s’ mouse with near-normal functional measurements recorded at more than 70 days.
 4:57 PM
4:57 PM
 Keshav Bhat
Keshav Bhat





















