Tuesday, June 22, 2010
Friday, June 18, 2010
Medicare Could Save $500 Million By Switching Drugs For AMD Treatment


After examining data on some 200,000 patients on Medicare, researchers found that expenditures for Avastin averaged about $42 per dose per eye, compared to $1,593 for a dose of Lucentis.
These study results have not yet been submitted to a medical journal for peer review, a fact that troubles Sen. Herb Kohl (D-WI), who chairs the Senate Committee on Aging. Kohl stated, "It is baffling that CMS would delay the release of this data when there are hundreds of millions of taxpayer dollars at stake.
High HbA1c in Black compared with White people may falsify diabetes testing
Black individuals with diabetes and prediabetes have previously been shown to have higher levels of HbA1c than their White counterparts. However, there are little available data on links between ethnicity and HbA1c in nondiabetic individuals.
To investigate further, David Ziemer (Emory University, Atlanta, Georgia, USA) and colleagues recruited 1581 and 1967 non-Hispanic Black and White individuals without known diabetes from the SIGT (Screening for Impaired Glucose Tolerance) study and the NHANES III (Third National Health and Nutrition Examination) survey, respectively.
As reported in the Annals of Internal Medicine, the team found that HbA1c levels were 0.13% and 0.21% higher in Black than White participants with normal glucose tolerance (fasting plasma glucose [FPG] below 100 mg/dl) in the SIGT and NHANES III groups, respectively.
To investigate further, David Ziemer (Emory University, Atlanta, Georgia, USA) and colleagues recruited 1581 and 1967 non-Hispanic Black and White individuals without known diabetes from the SIGT (Screening for Impaired Glucose Tolerance) study and the NHANES III (Third National Health and Nutrition Examination) survey, respectively.
As reported in the Annals of Internal Medicine, the team found that HbA1c levels were 0.13% and 0.21% higher in Black than White participants with normal glucose tolerance (fasting plasma glucose [FPG] below 100 mg/dl) in the SIGT and NHANES III groups, respectively.
Tuesday, June 15, 2010
Role of Diet & Medications in Cataract Development
Two studies published in the June issue of the Archives of Ophthalmology, healthy diet helps guard against cataracts, while certain medications raise the risks of this common cause of vision loss.
In the first study, involving 1,808 middle-aged and elderly women, researchers found that those who eat foods that contain high levels of a variety of vitamins and minerals may be less likely to develop nuclear cataract.
A second study found that medications that increase sensitivity to the sun -- including antidepressants, diuretics, antibiotics, and the pain reliever naproxen sodium (commonly sold over-the-counter as Aleve) -- increase the risk of age-related cataract.
Higher prevalence of cataracts in women was also associated with other modifiable factors, such as smoking and obesity, and with nonmodifiable factors, such as brown eyes, myopia, and high pulse pressure, MedPage Today reported. Still, diet was the strongest risk factor related to reduced risk of nuclear cataract in this sample of postmenopausal women, the study authors noted, adding, "Lifestyle improvements that include healthy diets, smoking cessation, and avoiding obesity may substantively lower the need for and economic burden of cataract surgery in aging American women".
In the first study, involving 1,808 middle-aged and elderly women, researchers found that those who eat foods that contain high levels of a variety of vitamins and minerals may be less likely to develop nuclear cataract.
A second study found that medications that increase sensitivity to the sun -- including antidepressants, diuretics, antibiotics, and the pain reliever naproxen sodium (commonly sold over-the-counter as Aleve) -- increase the risk of age-related cataract.
Higher prevalence of cataracts in women was also associated with other modifiable factors, such as smoking and obesity, and with nonmodifiable factors, such as brown eyes, myopia, and high pulse pressure, MedPage Today reported. Still, diet was the strongest risk factor related to reduced risk of nuclear cataract in this sample of postmenopausal women, the study authors noted, adding, "Lifestyle improvements that include healthy diets, smoking cessation, and avoiding obesity may substantively lower the need for and economic burden of cataract surgery in aging American women".
Friday, June 11, 2010
Eye Exam May Spot Multiple Sclerosis
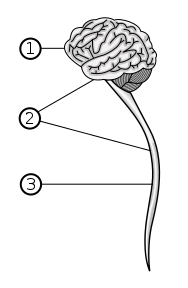 Image via Wikipedia
Image via Wikipedia
This technique has the potential to provide a powerful and reliable assessment strategy to measure structural changes in the central nervous system," study co-senior author Dr. Elliot Frohman, professor of neurology and ophthalmology and director of the Multiple Sclerosis Clinical Center at UT Southwestern, said in a medical center news release.
The study appears in the June issue of the journal Annals of Neurology. The research was a joint project with the University of Pennsylvania School of Medicine, John Hopkins University School of Medicine, and the University of Alabama at Birmingham
Avastin "Superior To Standard Care" For Treating Wet AMD, Researchers Say
A cheap drug used to treat bowel cancer should also be prescribed to patients with a condition that leads to sight loss, say UK researchers. Researchers at three eye centres in London, Bristol and Cheltenham carried out a pilot study in 131 patients with wet AMD.
The drug firm, Roche, which markets Avastin, has not applied for the drug to be used for wet AMD.
Barbara McLaughlan, RNIB campaigns manager for eye health and social care, said patients should continue to be treated with Lucentis until "robust evidence" was available on the safety and effectiveness of Avastin.
The drug firm, Roche, which markets Avastin, has not applied for the drug to be used for wet AMD.
Barbara McLaughlan, RNIB campaigns manager for eye health and social care, said patients should continue to be treated with Lucentis until "robust evidence" was available on the safety and effectiveness of Avastin.
Friday, June 04, 2010
 Image via Wikipedia
Image via Wikipedia
Their method, published recently in Journal of Neuroscience Methods, offers a potential new source of cells for retinal transplants. Specifically, the scientists created two types of cells from the human embryonic stem cells: early-stage retinal cells, and retinal pigment epithelium cells, which provide nourishment to the cells responsible for vision in the retina.
Robert Lanza, chief scientific officer at Advanced Cell Technologies, who was not involved in the study, says that his team discovered several years ago that, when turning human embryonic stem cells into RPE cells, other stem cells would spontaneously form layers, including patches of photoreceptors.
Monday, May 17, 2010

A new technique, developed by scientists at ARC Vision Centre and Australian National University (ANU), can quantify damage caused by serious eye diseases.
Called multifocal pupillography, the method involves monitoring minute responses of the eye's pupil to light signals in different parts of the patient's visual field.
ARC Vision Centre and Australian National University (ANU) researchers led by Ted Maddess and Andrew James are pioneering this area of study for painless detection and monitoring of glaucoma, age-related macular degeneration (AMD) and diabetic retinopathy.
The technique relies on a feedback loop of nerve signals, which flow from each eye to the brain and back again to both pupils of the eyes by a secondary pathway, Maddess explains.
In our research we have been trying to localise the responses of the pupil to particular places across the visual field and hence, the eye's retina, said Maddes.
Thursday, May 13, 2010
Artificial implants better than Laser Surgery
The UK's Guardian reported that, according to research published in the May issue of the Cochrane Database of Systematic Reviews, artificial lenses implanted inside the eye may be safer than laser surgery when it comes to improving short sightedness.
After performing a literature review of studies involving laser surgery or implantation of phakic intraocular lenses (IOLs) for the treatment of myopia, researchers from the Moorfields Eye Hospital in London found that both operations worked equally well to improve people's vision. The proportion of people who had 20/20 vision without wearing glasses, one year after surgery, was the same.
Implantation of phakic IOLs involves the insertion of a thin plastic lens inside the eye, either behind the pupil or in front of the iris, as opposed to laser surgery in which part of the cornea is cut away. Both operations work in the same way, however, changing how light enters the eye, bringing images into focus in the right place. The review examined the results from three trials, involving 132 patients, comparing the two types of operations.
MedPage Today reported, Safety, expressed in terms of loss of lines from pretreatment, best-corrected visual acuity, showed statistically significant differences in favor of IOLs for two of four outcomes. The review's authors suggested that phakic IOLs are safer than excimer laser surgical correction for moderate to high myopia in the range of -6.0 to -20.0 diopters [D], and phakic IOLs are preferred by patients, They added, While phakic IOLs might be accepted clinical practice for higher levels of myopia (greater than or equal to 7.0 D of myopic spherical equivalent with or without astigmatism), it may be worth considering phakic IOL treatment over excimer laser correction for more moderate levels of myopia.
After performing a literature review of studies involving laser surgery or implantation of phakic intraocular lenses (IOLs) for the treatment of myopia, researchers from the Moorfields Eye Hospital in London found that both operations worked equally well to improve people's vision. The proportion of people who had 20/20 vision without wearing glasses, one year after surgery, was the same.
Implantation of phakic IOLs involves the insertion of a thin plastic lens inside the eye, either behind the pupil or in front of the iris, as opposed to laser surgery in which part of the cornea is cut away. Both operations work in the same way, however, changing how light enters the eye, bringing images into focus in the right place. The review examined the results from three trials, involving 132 patients, comparing the two types of operations.
MedPage Today reported, Safety, expressed in terms of loss of lines from pretreatment, best-corrected visual acuity, showed statistically significant differences in favor of IOLs for two of four outcomes. The review's authors suggested that phakic IOLs are safer than excimer laser surgical correction for moderate to high myopia in the range of -6.0 to -20.0 diopters [D], and phakic IOLs are preferred by patients, They added, While phakic IOLs might be accepted clinical practice for higher levels of myopia (greater than or equal to 7.0 D of myopic spherical equivalent with or without astigmatism), it may be worth considering phakic IOL treatment over excimer laser correction for more moderate levels of myopia.
Phakic IOLs May Be Safer Than Laser Surgery For Myopia
The UK's Guardian reported that, according to research published in the May issue of the Cochrane Database of Systematic Reviews, artificial lenses implanted inside the eye may be safer than laser surgery when it comes to improving short sightedness.
After performing a literature review of studies involving laser surgery or implantation of phakic intraocular lenses (IOLs) for the treatment of myopia, researchers from the Moorfields Eye Hospital in London found that both operations worked equally well to improve people's vision. The proportion of people who had 20/20 vision without wearing glasses, one year after surgery, was the same.
Implantation of phakic IOLs involves the insertion of a thin plastic lens inside the eye, either behind the pupil or in front of the iris, as opposed to laser surgery in which part of the cornea is cut away. Both operations work in the same way, however, changing how light enters the eye, bringing images into focus in the right place. The review examined the results from three trials, involving 132 patients, comparing the two types of operations.
MedPage Today reported, Safety, expressed in terms of loss of lines from pretreatment, best-corrected visual acuity, showed statistically significant differences in favor of IOLs for two of four outcomes. The review's authors suggested that phakic IOLs are safer than excimer laser surgical correction for moderate to high myopia in the range of -6.0 to -20.0 diopters [D], and phakic IOLs are preferred by patients, They added, While phakic IOLs might be accepted clinical practice for higher levels of myopia (greater than or equal to 7.0 D of myopic spherical equivalent with or without astigmatism), it may be worth considering phakic IOL treatment over excimer laser correction for more moderate levels of myopia.
After performing a literature review of studies involving laser surgery or implantation of phakic intraocular lenses (IOLs) for the treatment of myopia, researchers from the Moorfields Eye Hospital in London found that both operations worked equally well to improve people's vision. The proportion of people who had 20/20 vision without wearing glasses, one year after surgery, was the same.
Implantation of phakic IOLs involves the insertion of a thin plastic lens inside the eye, either behind the pupil or in front of the iris, as opposed to laser surgery in which part of the cornea is cut away. Both operations work in the same way, however, changing how light enters the eye, bringing images into focus in the right place. The review examined the results from three trials, involving 132 patients, comparing the two types of operations.
MedPage Today reported, Safety, expressed in terms of loss of lines from pretreatment, best-corrected visual acuity, showed statistically significant differences in favor of IOLs for two of four outcomes. The review's authors suggested that phakic IOLs are safer than excimer laser surgical correction for moderate to high myopia in the range of -6.0 to -20.0 diopters [D], and phakic IOLs are preferred by patients, They added, While phakic IOLs might be accepted clinical practice for higher levels of myopia (greater than or equal to 7.0 D of myopic spherical equivalent with or without astigmatism), it may be worth considering phakic IOL treatment over excimer laser correction for more moderate levels of myopia.
Tuesday, May 11, 2010
A great series of tutorials
Here is a video that describes the theory and practical use of Goldman Tonometry. Excellent resource for pre-testing staff and for students.
Monday, May 10, 2010
Friday, May 07, 2010
Idiopathic Intracranial Hypertension May Cause Vision Loss

Idiopathic intracranial hypertension (IIH), also known as pseudotumor cerebri, is an unexplained buildup of fluid in the brain that pushes on the optic nerve, often causing headaches, vision loss, or even blindness. Some people with the condition may report visual problems, nausea, and tinnitus.
Interestingly, the majority of patients who develop pseudotumor cerebri are obese, although the link is not well understood. Dr. Steve Roach, chief of neurology and vice chair of pediatrics at Nationwide Children's Hospital in Columbus, Ohio is part of a team of doctors who opened up the first center dedicated to treating children with pseudotumor cerebri.
IIH can be controlled by weight loss and medication. To slow the loss of vision, a procedure called optic nerve fenestration can be done; which leaves a small window in the sheath of the optic nerve to release pressure.
Monday, May 03, 2010
How do blind people ski?
Visually impaired ski racer Danelle D'Aquanni Umstead:
My guide, Rob, always will ski in front so he can tell me what is coming up in the course, and what I may feel as we are skiing down it. We wear headsets that are an open line of communication between the two of us. This allows Rob to continue speaking to me and coaching me as we race down
Latino Americans Have Higher Rates Of Blindness, Diabetic Eye Disease, Cataracts
According to four papers published in the May issue of the American Journal of Ophthalmology, "Latino Americans have higher rates of visual impairment, blindness, diabetic eye disease, and cataracts than whites in the United States."
In analyzing data from more than 4,600 participants in the Los Angeles Latino Eye Study (LALES), researchers found that the Latinos' rates of visual impairment and blindness were the highest of any ethnic group in the country, compared to other US studies of different populations.
"These data have significant public health implications and present a challenge for eye care providers to develop programs to address the burden of eye disease in Latinos," Dr. Paul A. Sieving, director of the National Eye Institute, said in the news release.
In analyzing data from more than 4,600 participants in the Los Angeles Latino Eye Study (LALES), researchers found that the Latinos' rates of visual impairment and blindness were the highest of any ethnic group in the country, compared to other US studies of different populations.
"These data have significant public health implications and present a challenge for eye care providers to develop programs to address the burden of eye disease in Latinos," Dr. Paul A. Sieving, director of the National Eye Institute, said in the news release.
Tuesday, April 27, 2010
Systems To Help Blind See Again

Venture Capital Dispatch blog of the Wall Street Journal reported that two companies are working on vision systems to help some blind people see again.
Second Sight Medical Products, Inc. based in Sylmar, Calif. is developing special eyeglasses that transmit pictures to a receiver embedded on the retina. The images are transferred by the optic nerve to the brain. The device is targeted to patients who have lost most of their vision as a result of retinal degeneration and whose nerve connections are still intact.
Israel's Nano Retina Inc. is also developing a similar device. The devices are priced from $50,000 to $100,000. Both companies are now working with insurance companies to have them pick up the costs for patients in need of such devices.
A third company, Optobionics Corp is pursuing a trickier and more costly approach: restoring function to the damaged retina by using the device to stimulate the rods and cones, rather than using the system as an adjunct to the retina. They are looking for funds to enter Phase III trials.
Thursday, April 22, 2010
VA Rehab Center For Blinded Veterans To Be Named After Fallen Optometrist

A new rehab center for blinded service members will be named after Maj. Charles Robert Soltes Jr who was killed by a suicide bomber in Iraq.
The center is scheduled to be open in Long Beach next spring.
The bill to authorize that name was introduced by Rep. John Campbell, R-Irvine. Last month, it passed the House 417-0 and on Monday, April 19, it passed the Senate without the need for a roll call vote.
On Monday evening, Sen. Daniel Akaka, D-Hawaii, chairman of the Veterans Affairs Committee, spoke up for the measure.
"Major Soltes was a dedicated Army officer and an outstanding clinician, educator and military optometrist,'' Akaka said. "And naming the Long Beach VA blind rehabilitation center in honor of him will be a fitting tribute to his lasting memory.''
Wednesday, April 21, 2010
Early Screening For Type 2 Diabetes Cost Effective

According to a study published online March 30 in The Lancet, early screening for type 2 diabetes is cost effective and prevents diabetes-related complications, including myocardial infarction and blindness.
By using mathematical modeling to assess several screening strategies, researchers determined the most cost-effective approach is to begin screening patients for type 2 diabetes between ages 30 and 45, with follow-up every three to five years. They arrived at this conclusion by studying a simulated population of 325,000 non-diabetic 30-year-olds using the National Health and Nutrition Examination Survey data from 1999 through 2004.
Monitoring May Be Enough For Some Patients At Risk For Glaucoma
Dallas Morning News reported that most patients who are at risk of developing glaucoma because of high eye pressure may just require monitoring.
In a 15-year study presented at the American Glaucoma Society's annual meeting and published in the Archives of Ophthalmology, participants with elevated eye pressure but no evidence of glaucoma were randomized to eye drops or were simply monitored.
In the second part of the study, during which all participants received eye drops, researchers found that in lower-risk patients there was not much difference between those taking drops the whole time and those who got drops seven years later.
In a 15-year study presented at the American Glaucoma Society's annual meeting and published in the Archives of Ophthalmology, participants with elevated eye pressure but no evidence of glaucoma were randomized to eye drops or were simply monitored.
In the second part of the study, during which all participants received eye drops, researchers found that in lower-risk patients there was not much difference between those taking drops the whole time and those who got drops seven years later.
Tuesday, April 20, 2010
You thought contact lenses are to correct vision?

The UK's Daily Mail reports that thanks to advances in technology, contact lenses have been "transformed...into valuable health tools" that do more than just correct vision.
For example,
Red-tinted contact lenses have been developed to relieve the agony of migraines. They work by filtering out wavelengths of light that over-stimulate retinal receptors - lightsensitive tissues lining the inner surface of the eye - which results in head pain.
Researchers at the University of Western Ontario, Canada, have created lenses that chemically react to glucose found in tears as a means of monitoring glucose levels in diabetics.
 11:09 AM
11:09 AM
 Keshav Bhat
Keshav Bhat






![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=2663f600-5338-4347-a3e2-a927400f4d36)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=35dacee8-f0fe-498c-9017-64dc59dd4cfb)

![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=31a3472f-26ad-48be-949d-f0ea376a47a2)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=f43462ee-82cd-448e-9069-3d008ad2736b)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=7b4fe8e8-7f62-4b20-8554-8db4d37d7bff)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=27cac58e-5b4d-47df-a084-8038b32ef248)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=3c18d108-1d43-451c-9084-6506c53da1b6)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=ca760e04-9f39-40a1-9b19-19097bea9c5c)



